A dangerous myth about illicit fentanyl, the opioid largely behind the surge in overdose deaths, simply will not die. While addiction and drug policy experts have repeatedly refuted the idea that touching fentanyl alone can cause an overdose, like a stubborn weed, the lie keeps coming back. And now the myth has drifted upward to policymakers, who are ignoring the lack of evidence that mere exposure to fentanyl can be deadly.
At this moment, three bills — one in Florida (SB 718), one in West Virginia (HB 5319) and the other in Tennessee (SB 1754) — are making their way through their respective state legislatures. All three will allow for a felony charge to be levied against people who expose a first responder to fentanyl or a fentanyl analog, such as carfentanil or remifentanil. But HB 5319 casts an even wider net, encompassing any opioid regardless of potency.
In all of the bills, the language is broad, allowing for routes of exposure to include touch, inhalation and ingestion. And very critically, while HB 5319 does include language which would require a laboratory test for opioids be administered to the first responder in question, SB 718 and SB 1754 do not.
Specifically, Florida’s SB 718 allows for criminal penalties to be levied against people who “recklessly expose first responders to fentanyl, fentanyl derivatives, analogs of fentanyl, or mixtures containing such substances and an overdose or serious bodily injury of a first responder results.”
As deadly as fentanyl can be, touching it or being merely exposed to it is just not a threat. That’s not how fentanyl works.
Tennessee’s SB 1754 would allow for aggravated assault against a first responder charges against anyone who “knowingly possesses fentanyl, carfentanil, remifentanil, alfentanil, or thiafentanil in a manner that would be reasonably foreseen to expose a first responder to the substance while the first responder is discharging or attempting to discharge the first responder's official duties and the first responder is exposed to the substance.”
And West Virginia’s HB 5319 is similar, levying a felony charge against anyone exposing first responders “to opioids,” resulting in any one of an ill-defined array of effects, including “any impairment of physical condition.”
These bills probably seem innocuous, perhaps even necessary — why shouldn’t we want to protect first responders from a substance involved in the deaths of hundreds of thousands of people over the last two decades?
Because as deadly as fentanyl can be, touching it or being merely exposed to it is just not a threat. That’s not how fentanyl works. And yes, this distinction matters.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter Lab Notes.
Fentanyl is indeed a very potent opioid, meaning that its effects, such as pain relief and euphoria, are felt with only a relatively small dose. In the context of hospitals and ambulances — where fentanyl is safely used every day without incident — the drug is dosed in micrograms, orders of magnitude smaller than the more familiar milligram.
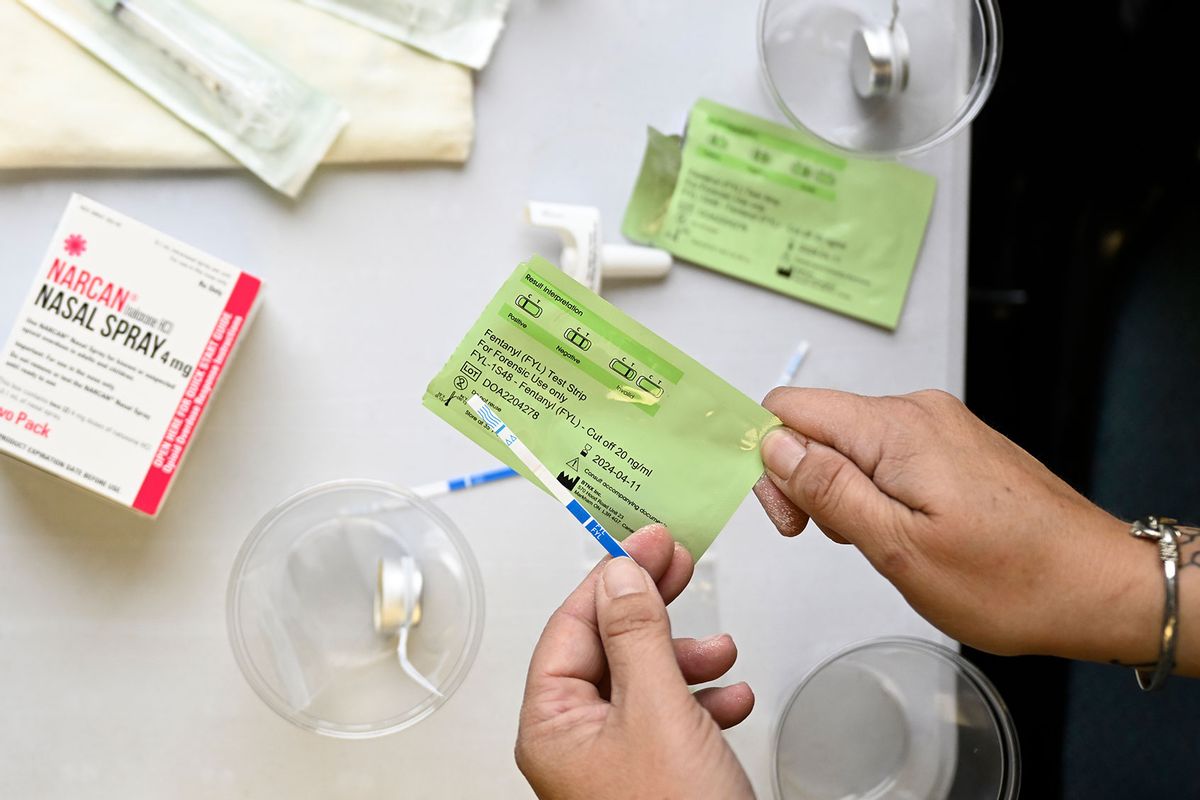
It’s this high degree of potency that makes it deadly for people who use unregulated drugs, because unlike the clinical context for pharmaceutical fentanyl, where we can dose and administer very precise amounts of drugs to patients, the unregulated fentanyl in the illicit supply offers no such insight. People using drugs are often caught unaware and by surprise at the presence or amount of fentanyl in their supply. And without having someone nearby, armed with the opioid overdose reversing drug naloxone, this is frequently a fatal situation.
But while fentanyl is easily absorbed through injection, pyrolyzing and inhaling its vapor, snorting it or swallowing it, it isn’t good at passing through skin. When it hit the market in the 1990s, Duragesic, the trade name for the fentanyl skin patch, was a minor marvel of drug delivery innovation precisely for this reason. It took many years of effort to develop and refine a way to move fentanyl across the skin, much less in a controlled and predictable way. And even then, reaching a steady, pain-relieving blood concentration of fentanyl with the patch takes several hours, even with sustained contact. Fentanyl also does not aerosolize on its own, which is why people have to either snort (i.e., insufflate rather than inhale) or intentionally vaporize it.
If the science here is so straightforward, why is there still confusion? This myth of passive fentanyl overdose was first put forth in a 2016 bulletin from the Drug Enforcement Agency, which has since been updated, and the language softened. Other authoritative bodies like the CDC have repeated the myth, and despite changing their warnings to reflect the fact that there is no evidence this can happen or has ever happened, the agency still maintains a rather misleading guide under NIOSH’s website, which largely deals in hypothetical situations that are very unlikely to ever happen.
The more likely explanation is an anxiety reaction or a similar psychosomatic response, like the “nocebo effect.”
But if you’ve been following headlines, this all may be a surprise to you. Over the years, we’ve seen a steady drip of pieces on police encounters with fentanyl resulting in alleged overdoses. The more peripheral details vary, but the core remains strikingly consistent — an officer saw something that looked like a drug, or perhaps dusted some powdery grains off of their uniform. Someone mentions fentanyl. Suddenly they feel something — heart pounding, chest tightening, fingers tingling, light-headedness. Often, these officers are able to give themselves naloxone, the antidote to an opioid overdose. And while these experiences are certainly frightening, they aren’t opioid overdoses, which cause slow or absent breathing and a loss of consciousness.
Despite their viral spread in media and online, the smallest amount of scrutiny is able to disprove every single instance. The more likely explanation is an anxiety reaction or a similar psychosomatic response, like the “nocebo effect” (essentially the opposite of the placebo effect), where simply believing something can harm you will cause very real symptoms. We can, indeed, convince ourselves that boogeymen are real. Who among us hasn’t jumped at every small noise after watching a scary movie alone at night? But ultimately, we must separate myth from fact. Especially when, as is the case here, the myth actively harms others.
We already know that increased criminal justice involvement makes it harder, not easier, for people who use drugs to have a bright future, or any future at all. Release from jail or prison is well-known to be a factor in significant overdose risk. And despite common rhetoric to the contrary, drugs are commonly accessible to incarcerated people, bursting the oft-cited “you can get sober inside” bubble.
With a drug conviction on one’s record, it becomes monumentally more difficult to get an apartment, a job or access a litany of social services which would be of considerable use to someone exiting incarceration. And these are the easily tracked consequences, which say nothing of the stigma and shame carried with a criminal record, especially one related to drug use. Simply put, we have already set these people up to fail. And now Tennessee, West Virginia and Florida are about to make it even easier — without any scientific or logical justification — to further hobble their citizens who use drugs.
And unfortunately, these bills represent a worrying inflection point for American drug policy, such as Idaho banning their syringe access programs in defiance of decades of scientific precedent or Oregon’s legislature overturning the will of voters by repealing Measure 110, which treated drug possession as a health problem instead of a criminal one.
We need your help to stay independent
The underground nature of illicit drug markets make them ripe for misinformation and rumors. While passive fentanyl exposure myths have been a stubborn fixture in recent years, this is the first time since the start of the overdose epidemic that such a thoroughly disproven fentanyl myth has been weaponized into legislation. Moving towards effective drug policy requires, at minimum, laws and policies based in reality. These bills not only miss that mark, but if they pass, will wield this myth like a cudgel against their own people.
Additionally, while the evidence behind these bills is nonexistent, this is not the message received by the public. A law stating that first responders are in need of extraordinary protection from contacting fentanyl says that passive overdose risk is real, and would necessarily apply to anyone. Even before these bills were written, anxiety about potential risks of touching someone who is experiencing an overdose has threatened timely bystander response to opioid overdose. What we desperately need is more community response to overdose, not less.
Rampant and stubborn mythologies about the contact risks of fentanyl have already created confusion and anxiety in the American public. People need fact-based education about real risks, rather than worrying about fantastical narratives which only stir up panic. At the very least, we can choose not to codify this fiction into laws that will further harm people who use drugs, while protecting no one.


Shares